COVID-19 has pummelled Kenya’s economy and upended social life, and the president is under immense pressure to lift the curfew and ease other containment measures. The scope and scale of disruption and uncertainty caused by the virus have never been witnessed in Kenya before; and this could conceivably explain the dissonant voices among policymakers on good practices in containing the infections as well as reopening the country. As the country inches closer to an inevitable resumption – a new normal – the government could find value in two key policy imperatives: mitigation against the risk of a new surge of infections (or second wave) and well hashed out non-pharmaceutical interventions.
Initial epidemiological projections indicated that Kenya will record 1,000 COVID-19 cases by mid-April and a further 4,000 cases a week later. However, these grim projections did not come to pass. By the end of April, the Ministry of Health had reported just under 400 total cases. Numerous hypotheses for the ‘low’ numbers have been advanced and deliberated extensively. These range from the late arrival of the virus in the country, extensive experience in handling highly communicable diseases such as Bacille Calmette-Guérin (BCG), a youthful population, limited international travels, to a lack of adequate testing equipment and mass testing, among others. The jury is still out on the veracity of these claims. Often left out in the deliberations are the government’s aggressive initiatives such as curfews, directives on the use of protective equipment, border closures, and other travel restrictions.
So far, some gains have been made against the pandemic, but the battered economy is about to go bust, and health practitioners and economists alike (in their own ways) are gravely concerned about the future. The ineluctable reopening of the country should then come with a great measure of discipline and order to mitigate ‘second wave’ of infections (understood as the period following the reopening). The second wave (s) of the Spanish flu in 1918; H1N1 epidemic in 2009; and now COVID-19 in Singapore and South Korea ought to be vital lessons for decision makers. In all the above cases, the diseases worsened thanks to public health policy failures and mutation of the virus. The second wave in Kenya can be avoided, but the country must be prepared.
Mitigating a ‘second wave’ of infections
From mass testing that began in early May, the daily average number of infected confirmed cases is a cause for concern. Inferring from these statistics, there are more than enough number of infected and highly susceptible people who can trigger a second wave of infections. A new study shows that 10 per cent of infected individuals could potentially cause 80 per cent of new cases. Add that to the likely impact of ‘super spreaders’ in the country if measures are lifted – think of schools, crowded nightclubs and bars, informal settlements, and of course, socio-cultural events such as weddings and funerals. Left unchecked, it could be cataclysmic for a stretched health system.
Given the foregoing, therefore, decision makers should be preoccupied with creating near-hermetic policies that will prevent higher infection rates upon resumption. The Ministry of Health ought to adopt a proven epidemiological model. But this is not enough. A functional model is as good as extrapolated data. In the past, for instance, Susceptible-Exposed-Infected-Recovered (SEIR) model has been used successfully in predicting the spread of highly infectious diseases such as SARS, Ebola, Zika; and more recently, COVID-19 in Wuhan, China. The success of this model in these situations has been attributed to accurate data and timely reporting. It is also worth noting that sound health-related policies are corollaries of well-designed epidemiological modelling, and without correct numbers, the policies are bootless. This is why Afya House needs to get them right and in good time.
Other critical fundamentals include adequate testing equipment, enhanced countrywide mass testing, more efficient contact tracing, and a well-resourced healthcare system that prioritizes doctors and nurses. In Sun Tzu words, ‘one must know oneself and one’s enemy’ in order to succeed in war. Case in point; do authorities fully understand the transmissibility and severity of COVID-19 in the country? What about the country’s fragilities and idiosyncrasies such as mannerism and conduct? If these questions are correctly answered, half the problem will have been resolved, and a second wave averted.
Non-pharmaceutical initiatives
Outside these interventions, the country should enhance hitherto relatively effective non-pharmaceutical initiatives to avoid new COVID-19 explosions. The zeal and vigor in containing the spread of the virus witnessed since March 13, 2020 should only be a primer to more stringent measures but which should not fundamentally hurt the already hobbling economy. The curfew and limited travel restrictions can be readjusted with strict guidelines on protective measures. While it will be difficult to control human density in some areas, including informal settlements through social distancing, the mandatory wearing of masks or glass shields, washing hands, temperature screening at entry points, and use of sanitizer spray booths should be ‘categorical imperatives’ in all sectors for as long as new infections are reported. This is the price Kenyans will have to pay for reopening.
The much-hyped phased reopening strategy should also prioritize vital segments of the economy but policymakers should note that there is ubiquitous complementarity in Kenya’s economy. These include transport, tourism, agriculture, and manufacturing. The partial reopening of certain sectors would have knock-on effects on others, and thus the risk of not realizing the full potential of reopening the country. The best way is to have joint collaborative committees from each sector working in accord to have one comprehensive and coherent strategy.
With these measures in place, all Kenyans should pull together and demonstrate a sense of social responsibility by practising good hygiene and protecting the lives of the vulnerable. The country is in a precarious position of trying to balance health with economic costs brought forth by the pandemic. Therefore, as the country prepares for possible relaxation of current restrictions in the near future, by all means, everyone should stay up to speed on the patterns of the pandemic in the country and carry out individual and collective duties to flatten the curve and stop second wave infections.
Daniel Iberi is the Strategic Communications Manager at the HORN Institute.
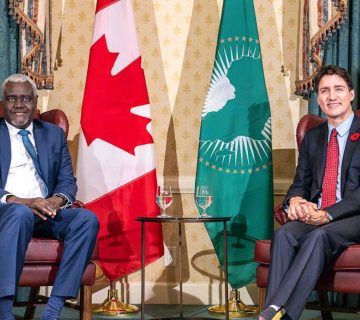
Photo: People stand in line for mass testing for COVID-19 in Kibera slum in Nairobi, Kenya on May 26, 2020 (Photo Credit: Reuters/Baz Ratner)